Future of healthcare brings community to church
 Dr. Wendy Wolf leads a forum on health care at the Congregational Church of Boothbay July 12. MORGAN CALLAN ROGERS/News Contributor
Dr. Wendy Wolf leads a forum on health care at the Congregational Church of Boothbay July 12. MORGAN CALLAN ROGERS/News Contributor
 Former legislator and policy director of Maine’s Consumers for Affordable Healthcare Steve Butterfield asks what problem the ACHA bill will solve. MORGAN CALLAN ROGERS/News Contributor
Former legislator and policy director of Maine’s Consumers for Affordable Healthcare Steve Butterfield asks what problem the ACHA bill will solve. MORGAN CALLAN ROGERS/News Contributor
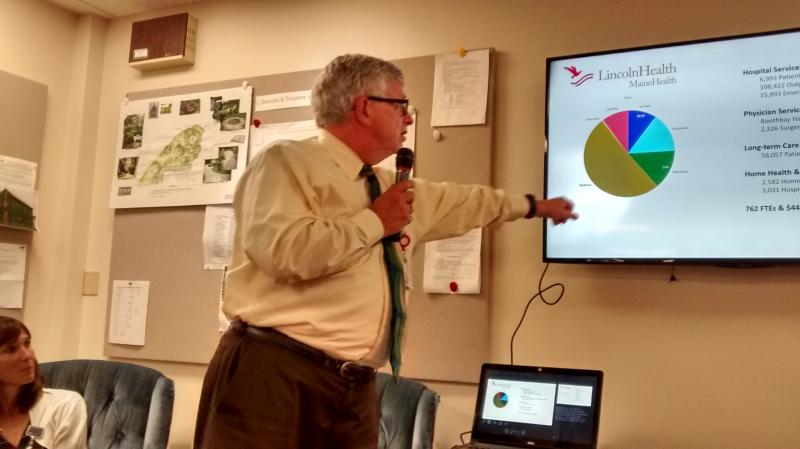 Dr. Wayne Printy, CFO of Lincoln County Health, speaks about the possible financial consequences to the region if the ACHA passes. MORGAN CALLAN ROGERS/News Contributor
Dr. Wayne Printy, CFO of Lincoln County Health, speaks about the possible financial consequences to the region if the ACHA passes. MORGAN CALLAN ROGERS/News Contributor
 Stacey Miller Friant, vice president for physician’s services for Lincoln County Health, is concerned about recruiting physicians and services into the region. MORGAN CALLAN ROGERS/News Contributor
Stacey Miller Friant, vice president for physician’s services for Lincoln County Health, is concerned about recruiting physicians and services into the region. MORGAN CALLAN ROGERS/News Contributor
 Dr. Wendy Wolf leads a forum on health care at the Congregational Church of Boothbay July 12. MORGAN CALLAN ROGERS/News Contributor
Dr. Wendy Wolf leads a forum on health care at the Congregational Church of Boothbay July 12. MORGAN CALLAN ROGERS/News Contributor
 Former legislator and policy director of Maine’s Consumers for Affordable Healthcare Steve Butterfield asks what problem the ACHA bill will solve. MORGAN CALLAN ROGERS/News Contributor
Former legislator and policy director of Maine’s Consumers for Affordable Healthcare Steve Butterfield asks what problem the ACHA bill will solve. MORGAN CALLAN ROGERS/News Contributor
 Dr. Wayne Printy, CFO of Lincoln County Health, speaks about the possible financial consequences to the region if the ACHA passes. MORGAN CALLAN ROGERS/News Contributor
Dr. Wayne Printy, CFO of Lincoln County Health, speaks about the possible financial consequences to the region if the ACHA passes. MORGAN CALLAN ROGERS/News Contributor
 Stacey Miller Friant, vice president for physician’s services for Lincoln County Health, is concerned about recruiting physicians and services into the region. MORGAN CALLAN ROGERS/News Contributor
Stacey Miller Friant, vice president for physician’s services for Lincoln County Health, is concerned about recruiting physicians and services into the region. MORGAN CALLAN ROGERS/News Contributor
A public forum on health care insurance brought 60 people into the Congregational Church in Boothbay Harbor on July 12. The three panelists were Dr. Wayne Printy, Lincoln County Healthcare chief financial officer, Steve Butterfield, former Maine legislator and current policy director for Maine’s Consumers for Affordable Healthcare, and Stacey Miller Friant, vice president of physicians’ services at Lincoln County Healthcare. Boothbay Region Community TV (BRCTV), Channel 7, filmed the event.
Dr. Wendy Wolf, Boothbay Harbor select board chair, organized the forum, which focused on differences between the Affordable Care Act (ACA, or Obamacare) and the American Health Care Act (AHCA) legislation currently moving through Congress. The AHCA, if passed, will abolish and replace Obamacare.
Wolf, a retired pediatric cardiologist, holds a degree from Harvard in public health and was the first president and CEO of the Maine Health Access Foundation. Wolf said one reason she went into public health was because she found it hard to work with uninsured patients as terrified of being bankrupted by an illness as they were by a potential diagnosis. “As a doctor, I believe it’s morally wrong to have people worried about finances when they’ve just received a new cancer diagnosis,” she said.
While Wolf believes Obamacare is superior to anything else she’s seen, she is concerned about the program’s long-term sustainability. “The problem is that it’s a giant tax transfer. We’re paying the federal government to provide financial help to people who can’t afford premiums,” she said. That money then is paid to insurance companies, and she wonders how enough will be generated to offset premiums as the cost of living rises.
Wolf introduced Butterfield first. He asked, “What problem is Congress trying to solve with the ACHA?” He believes Obamacare did a good job. He said the uninsured rate declined from 16.5 percent in 2013 to 10.5 percent in 2015. “In Maine, we’ve gone from 11 percent to 6 percent. Medical debt is no longer the major driver of personal bankruptcy,” he said, adding, if the proposed ACHA healthcare plan passes, it will eliminate current care granted to 24 million people.
Butterfield said the new plan would charge about 229,000 Mainers for their pre-existing conditions. He worries they would be priced out of the market. But, he told the audience, “There is one thing I want you to remember tonight. These bills are not about replacing Obamacare. They are radical overhauls of the Medicaid program.”
Medicaid will be significantly cut back over the next 20 years, Butterfield said. Currently, states pay their share, with a match from the federal government. Maine gets two dollars for every one paid into Medicaid. Proposed changes would give states a base rate per enrollees. That base amount will experience a slight rise on an annual basis; but because the cost of living will rise more, at about about the ten-year mark, the small Medicaid increases will level out. “That’s where you begin seeing a 35 percent cut to the program,” he said.
Printy spoke next. “It’s difficult to come up with specifics regarding a legislative proposal that changes every day,” he said. He focused his comments around rural health care and on Lincoln County.
He provided the audience with some of Lincoln Healthcare’s 2016 statistics, which included 7,000 patient days, 108,000 outpatient visits and 16,000 emergency and urgent care visits, which he said were typical for rural health care systems. “We also did 2,300 surgeries last year, saw 58,000 patient days in our long-term care facilities, 2,500 home health visits, and 3,000 hospice days.”
Last year, Lincoln County Healthcare racked up almost $9 million in uncompensated care, including free care for those eligible, and for unpaid bills. “This year, we’re projecting $9.4 million,” he said. When Maine opted out of a Medicaid expansion and cut qualifications, more patients were shunted into the self-pay and free-pay categories, along with patients unable to pay, Printy said. “Free care is a misnomer, because in the end, everybody else pays. So, even though you’re not one of those who have lost coverage in the cutback, you have a stake in it.”
Printy echoed Butterfield when he said that during the next 10 years, “We’re looking at an $834 billion cut in Medicaid. There will be a $120 billion shift from health care to general deficit reduction. Behavioral health will see impacts because it is funded through Medicaid. And this comes at a time when we’re experiencing significant problems in the area of drug and opioid abuse. This will devastate Maine.”
Maine law requires free care for citizens without insurance coverage, said Printy. “It’s going to be difficult to sustain current levels of operations with the bad debt that would result. We’re looking at a $35 million impact over a 10-year period,” he said.
The final panel member Wolf introduced, Friant, shared observations based on interactions with providers and patients.
“I do my best to recruit and retain all providers in Lincoln County. With rising costs due to uncompensated care, it is difficult for rural areas to bring in physicians to provide access to the services that we need. We’ve been actively recruiting for a physician for the Boothbay area for 18 months, but it’s difficult to pay competitive wages to physicians throughout Lincoln County. There is also a shortage of primary physicians training, and we are competing with the likes of Maine Medical Center,” Friant said.
“We feel fortunate to have the physicians who want to be here — they want to practice in rural Maine and we have been fortunate to keep them. But it’s difficult at this point to recruit and bring new members in,” she said.
The complete forum can be viewed on BRCTV.
Event Date
Address
United States