State officials cautiously optimistic over latest drug overdose data
As the number of Mainers dying from drug overdoses appeared to be going down in the first half of the year, recovery experts and state officials are increasingly looking to harm reduction strategies to aid efforts aimed at overdose prevention and treatment availability.
While “cautiously optimistic” that drug deaths are down this year — a decrease of about 6% for the first six months compared with the same period last year — there is still much to be done, said Gordon Smith, Gov. Janet Mills’ director of opioid response.
From January to May of this year, there were 253 confirmed and suspected fatal overdoses, according to the latest monthly overdose report from the Maine Office of the Attorney General and the University of Maine.
The June overdose report, not yet publicly available, will show that more than 300 people have died through June, Mills said at her fifth annual Opioid Response Summit in Portland last week.
Smith cautioned that it is too early to point to a trend or declare success, but the decrease in deaths remains significant considering that for the past four years Maine has seen a year-over-year increase in drug fatalities.
Still, the 723 deaths recorded last year were “too many,” Smith said.
“In a state with 1.3 million people, that is a lot of hardship and family agony and hurt. And it’s not acceptable to the governor or I,” he said.
The May overdose report shows that nonfatal overdoses in the first five months of the year were about level with the same period in 2022. Experts generally understand the actual number of nonfatal overdoses to be higher than the reported number because many overdoses may occur in private.
At last week’s summit, Mills introduced an updated strategic plan for Maine’s opioid response. Among other focus areas, the plan points to harm reduction as a critical strategy for reducing overdoses.
Harm reduction is a broad term that encompasses “evidence-based” approaches to engaging and equipping people who use drugs with “life-saving tools and information” to save lives and ultimately connect people with resources to set them on a path to long-term recovery, according to the Substance Abuse and Mental Health Services Administration.
It’s not clear what role harm reduction efforts in Maine played in this year’s decrease in drug deaths. But with the growing prevalence of contaminants in Maine’s illicit drug supply, programs such as the federal-grant funded Project DHARMA continue to be essential, Smith and other experts told The Maine Monitor.
Last summer, MaineHealth and several partner organizations launched Project DHARMA (“Distribution of Harm Reduction Access in Rural Maine Areas”) with the support of a $1.2 million, three-year federal grant. The grant is one of 25 SAMHSA awarded to organizations nationwide last year in a first-of-its-kind harm reduction grant program.
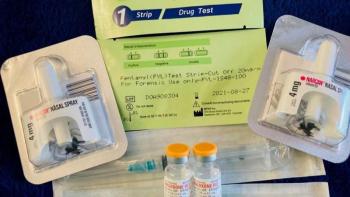
DHARMA is focused on expanding syringe service programs by embedding “harm reduction outreach specialists” in programs across the state. They will distribute safer use supplies, such as the opioid-overdose reversing drug naloxone, fentanyl test strips and clean syringes, as well as connect clients to treatment providers, the project’s directors said.
DHARMA is also working on training providers and students from a variety of disciplines, including medicine, dentistry and pharmacy, on topics ranging from how to prescribe pre-exposure prophylaxis, or PrEP, an antiretroviral therapy for HIV prevention, to discussions on the language and stigma surrounding substance use disorder in healthcare.
The first year of the project has mostly focused on the “logistics” of hiring the outreach specialists, who are the “heart of this grant,” said Dr. Kinna Thakarar, DHARMA’s lead researcher, and an infectious disease and addiction medicine physician at MaineHealth.
In the first two quarters of this year, the specialists had more than 6,000 “service encounters” with clients in the field or at “brick-and-mortar” locations statewide of syringe service programs, such as Church of Safe Injection, Maine Access Points and commonspace, Thakarar said.
“I think that has been one of the biggest accomplishments, and just seeing the collaboration among our syringe service program partners,” she said.
While that is well underway, another significant part of DHARMA, its drug checking program, had to overcome legal hurdles that required a legislative fix, according to Thakarar and Dr. Kristen Silvia, DHARMA’s medical director, and physician and director of the addiction medicine fellowship at MaineHealth.
DHARMA has partnered with Dr. Dasan Thamattoor, a chemistry professor at Colby College, and other academic partners to conduct drug checking, which is the process of “chemically (analyzing) street drug residue to understand what is actually in the local drug supply,” Thakarar said in testimony earlier this year.
Mills signed L.D. 1745, sponsored by Rep. Reagan LaRochelle, D-Augusta, into law late last month, which allowed “certain individuals” to possess, receive, transport or store “nominal amounts” of illicit or prescription controlled substances for the purposes of drug checking, LaRochelle testified.
Though there was an emergency preamble attached to the bill so that it went into effect immediately, the year-long setback means the drug checking program is still in preliminary stages, Silvia said.
Chasity Tuell, the Northern Maine Harm Reduction Director for Maine Access Points, said this program will be crucial because “with so many different contaminants, people don’t really know what they’re using.”
“Like they might have an idea of what they’re using but they don’t really know. And it’s hard to treat wounds if you don’t know what they’re from, it’s hard to detox off of something if you don’t know what you’re detoxing off of,” she said.
Thakarar said without the testing, it’s unclear what’s in the drug supply right now but “at this point, based on the wounds that we’re seeing and reports from the field, you know, xylazine is definitely in Maine.”
Xylazine is an animal tranquilizer that first appeared in toxicology reports in Maine in 2021, usually in combination with the synthetic opioid fentanyl. Not only is xylazine unresponsive to naloxone, it is not meant for human consumption and can cause necrotic wounds regardless of how it’s ingested, Silvia said.
“I think that’s why the drug checking program is going to be so helpful, because xylazine is not going to be the only contaminant, you know, that we see in this decade,” Thakarar said.
Fentanyl, which can be up to 50% more potent than heroin, continues to be present in about 70-80% of all drug deaths, according to overdose reports.
Mills announced at last week’s summit that her administration is using $1 million in federal funds to purchase and distribute xylazine test steps to syringe services providers, such as Tuell’s group.
DHARMA, via grants from the Office of Behavioral Health, is also looking to purchase handheld mass spectrometers for on-the-ground drug checking, Thakarar and Tuell said.
Tuell said she assumes there are other contaminants in the drug supply, such as another class of synthetic opioids called nitazenes, which Ohio Attorney General Dave Yost called “Frankenstein opioids” in a public health warning issued last year.
“But without being able to, like, really do comprehensive testing it’s hard to say for sure,” Tuell said.
“No one in the state is getting that information (right now) until really after a person dies and they do a toxicology.”